Blood
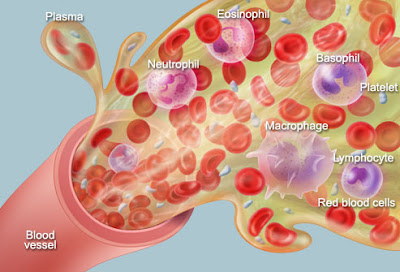
Blood is a constantly circulating fluid providing the body with nutrition, oxygen, and waste removal. Blood is mostly liquid, with numerous cells and proteins suspended in it, making blood "thicker" than pure water. The average person has about 5 liters (more than a gallon) of blood.
A liquid called plasma makes up about half of the content of blood. Plasma contains proteins that help blood to clot, transport substances through the blood, and perform other functions. Blood plasma also contains glucose and other dissolved nutrients.
About half of blood volume is composed of blood cells:
� Red blood cells, which carry oxygen to the tissues
� White blood cells, which fight infections
� Platelets, smaller cells that help blood to clot
Blood is conducted through blood vessels (arteries and veins). Blood is prevented from clotting in the blood vessels by their smoothness, and the finely tuned balance of clotting factors.
Blood Conditions
- Hemorrhage (bleeding): Blood leaking out of blood vessels may be obvious, as from a wound penetrating the skin. Internal bleeding (such as into the intestines, or after a car accident) may not be immediately apparent.
- Hematoma: A collection of blood inside the body tissues. Internal bleeding often causes a hematoma.
- Leukemia: A form of blood cancer, in which white blood cells multiply abnormally and circulate through the blood. The excessive large numbers of white cells deposit in the body's tissues, causing damage.
- Multiple myeloma: A form of blood cancer of plasma cells similar to leukemia. Anemia, kidney failure and high blood calcium levels are common in multiple myeloma.
- Lymphoma: A form of blood cancer, in which white blood cells multiply abnormally inside lymph nodes and other tissues. The enlarging tissues, and disruption of blood's functions, can eventually cause organ failure.
- Anemia: An abnormally low number of red blood cells in the blood. Fatigue and breathlessness can result, although anemia often causes no noticeable symptoms.
- Hemolytic anemia: Anemia caused by rapid bursting of large numbers of red blood cells (hemolysis). An immune system malfunction is one cause.
- Hemochromatosis: A disorder causing excessive levels of iron in the blood. The iron deposits in the liver, pancreas and other organs, causing liver problems and diabetes.
- Sickle cell disease: A genetic condition in which red blood cells periodically lose their proper shape (appearing like sickles, rather than discs). The deformed blood cells deposit in tissues, causing pain and organ damage.
- Bacteremia: Bacterial infection of the blood. Blood infections are serious, and often require hospitalization and continuous antibiotic infusion into the veins.
- Malaria: Infection of red blood cells by Plasmodium, a parasite transmitted by mosquitos. Malaria causes episodic fevers, chills, and potentially organ damage.
- Thrombocytopenia: Abnormally low numbers of platelets in the blood. Severe thrombocytopenia may lead to bleeding.
- Leukopenia: Abnormally low numbers of white blood cells in the blood. Leukopenia can result in difficulty fighting infections.
- Disseminated intravascular coagulation (DIC): An uncontrolled process of simultaneous bleeding and clotting in very small blood vessels. DIC usually results from severe infections or cancer.
- Hemophilia: An inherited (genetic) deficiency of certain blood clotting proteins. Frequent or uncontrolled bleeding can result from hemophilia.
- Hypercoaguable state: Numerous conditions can result in the blood being prone to clotting. A heart attack, stroke, or blood clots in the legs or lungs can result.
- Polycythemia: Abnormally high numbers of red blood cells in the blood. Polycythemia can result from low blood oxygen levels, or may occur as a cancer-like condition.
- Deep venous thrombosis (DVT): A blood clot in a deep vein, usually in the leg. DVTs are dangerous because they may become dislodged and travel to the lungs, causing a pulmonary embolism (PE).
- Myocardial infarction (MI): Commonly called a heart attack, a myocardial infarction occurs when a sudden blood clot develops in one of the coronary arteries, which supply blood to the heart.
Blood Tests
- Complete blood count: An analysis of the concentration of red blood cells, white blood cells, and platelets in the blood. Automated cell counters perform this test.
http://www.webmd.com/a-to-z-guides/complete-blood-count-cbc - Blood smear: Drops of blood are smeared across a microscope slide, to be examined by an expert in a lab. Leukemia, anemia, malaria, and numerous other blood conditions can be identified with a blood smear.
- Blood type: A test for compatibility before receiving a blood transfusion. The major blood types (A, B, AB, and O) are determined by the protein markers (antigens) present on the surface of red blood cells.
- Coombs test: A blood test looking for antibodies that could bind to and destroy red blood cells. Pregnant women and people with anemia may undergo Coombs testing.
- Blood culture: A blood test looking for infection present in the bloodstream. If bacteria or other organisms are present, they may multiply in the tested blood, allowing their identification.
- Mixing study: A blood test to identify the reason for blood being "too thin" (abnormally resistant to clotting). The patient's blood is mixed in a tube with normal blood, and the mixed blood's properties may provide a diagnosis.
- Bone marrow biopsy: A thick needle is inserted into a large bone (usually in the hip), and bone marrow is drawn out for tests. Bone marrow biopsy can identify blood conditions that simple blood tests cannot.
Blood Treatments
- Chemotherapy: Medicines that kill cancer cells. Leukemias and lymphomas are usually treated with chemotherapy.
- Blood transfusion: A blood donor's red blood cells are separated from their plasma and packed into a small bag. Transfusing the concentrated red blood cells into a recipient replaces blood loss.
- Platelet transfusion: A blood donor's platelets are separated from the rest of blood and concentrated into a plastic bag. Platelet transfusion is generally only performed when platelet counts fall to very low levels.
- Fresh frozen plasma: A blood donor's plasma (liquid blood) is separated from the blood cells, and frozen for storage. Plasma transfusion can improve blood clotting and prevent or stop bleeding that's due to clotting problems.
- Cryoprecipitate: Specific proteins are separated from blood and frozen in a small volume of liquid. Cryoprecipitate transfusion can replace specific blood clotting proteins when their levels are low, such as in people with hemophilia.
- Anticoagulation: Medicines to "thin" the blood and prevent clotting in people at high risk from blood clots. Heparin, enoxaparin (Lovenox) and warfarin (Coumadin) are the medicines most often used.
- Antiplatelet drugs: Aspirin and clopidogrel (Plavix) interfere with platelet function and help prevent blood clots, including those that cause heart attacks and strokes.
- Antibiotics: Medicines to kill bacteria and parasites can treat blood infections caused by these organisms.
- Erythropoietin: A hormone produced by the kidney that stimulates red blood cell production. A manufactured form of erythropoietin can be given to improve the symptoms of anemia.
- Bloodletting: In people with problems caused by too much blood (such as from hemochromatosis or polycythemia), occasional controlled removal of blood may be necessary.
